Maximizing Your PSHB CDHP: A Guide to Using Your Personal Care Account (PCA)
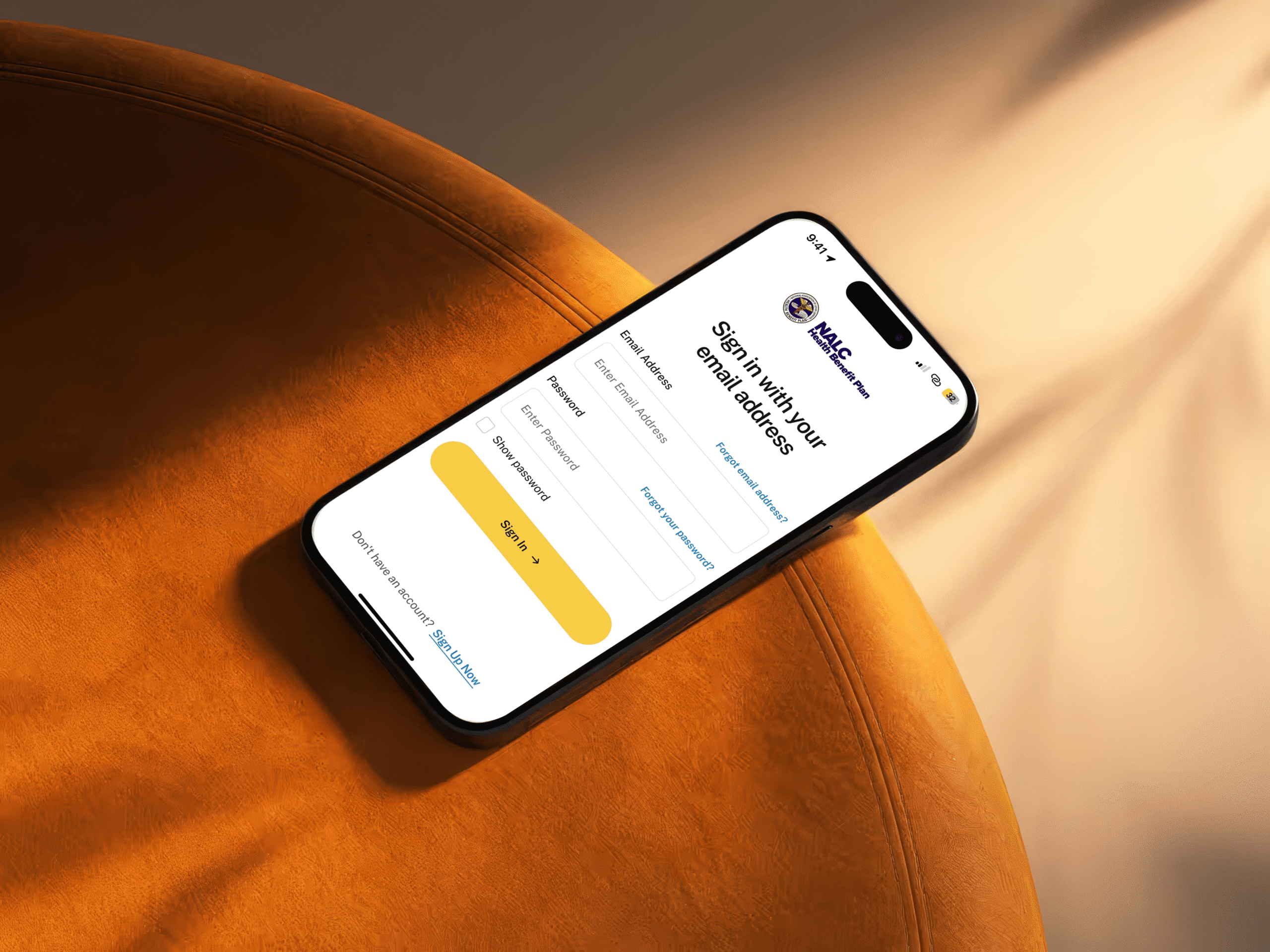
Navigating the complexities of healthcare plans can often feel overwhelming. However, the NALC HBP Consumer Driven Policy within the Postal Service Health Benefits program offers a unique feature that can make managing healthcare expenses simpler and more efficient: the Personal Care Account (PCA). In this guide, we’ll explore what a PCA is, how it benefits […]